[x_section style=”margin: 0px 0px 0px 0px; padding: 25px 0px 0px 0px; border-style: ridge; border-width: 1px 1px 1px 1px; “][x_row inner_container=”true” marginless_columns=”false” bg_color=”” style=”margin: 0px auto 0px auto; padding: 0px 0px 0px 0px; “][x_column bg_color=”” type=”1/1″ style=”padding: 0px 0px 0px 0px; “][x_text]Author: Dr. Adrian Zielinski
Reviewer & Edits: Dr. John Greenwood[/x_text][/x_column][/x_row][/x_section][x_section style=”margin: 0px 0px 0px 0px; padding: 0px 0px 0 0px; “][x_row inner_container=”true” marginless_columns=”false” bg_color=”” style=”margin: 0px auto 0px auto; padding: 0px 0px 0px 0px; “][x_column bg_color=”” type=”1/1″ style=”padding: 0px 0px 0px 0px; “][x_text]
Clinical Case
44 y/o M with a history of HTN presents to the ED after three days of productive cough and fevers.
On exam, the patient is lethargic, clammy, tachycardic, with crackles over the left upper lobe.
Vital signs are: Temp: 102.4, HR: 134, BP: 84/46, RR: 26, Sp02 84% on RA.
You astutely diagnose this patient with septic shock secondary to a pulmonary source and initiate fluid resuscitation and antibiotics. The blood pressure fails to respond after a 30cc/kg LR bolus, and you decide to initiate vasopressor therapy.[/x_text][/x_column][/x_row][/x_section][x_section style=”margin: 0px 0px 0px 0px; padding: 0px 0px 0px 0px; “][x_row inner_container=”true” marginless_columns=”false” bg_color=”” style=”margin: 0px auto 0px auto; padding: 0px 0px 0px 0px; “][x_column bg_color=”” type=”1/1″ style=”padding: 0px 0px 0px 0px; “][x_text]
What should be the first-line vasopressor in septic shock?
[/x_text][/x_column][/x_row][x_row inner_container=”true” marginless_columns=”false” bg_color=”” style=”margin: 0px auto 0px auto; padding: 0px 0px 0px 0px; “][x_column bg_color=”” type=”1/1″ style=”padding: 0px 0px 0px 0px; “][x_accordion][x_accordion_item title=”Answer” open=”false”]Pearl: Norepinephrine is the first choice vasopressor in septic shock
Norepinephrine has primarily α1 and β1 activity, with some β2 activity. It functions primarily to raise MAP by arterial constriction, with mild increase in inotropy, chronotropy, and venous return.[/x_accordion_item][/x_accordion][/x_column][/x_row][/x_section][x_section style=”margin: 0px 0px 0px 0px; padding: 0px 0px 0px 0px; “][x_row inner_container=”true” marginless_columns=”false” bg_color=”” style=”margin: 0px auto 0px auto; padding: 0px 0px 0px 0px; “][x_column bg_color=”” type=”1/1″ style=”padding: 0px 0px 0px 0px; “][x_text]
What is the correct timing to initiate vasopressor therapy?
[/x_text][x_accordion][x_accordion_item title=”Answer” open=”false”]Pearl: Early norepinephrine administration (<2 hours from the septic shock onset) is associated with decreased mortality compared to those who received it ≥2 hours after septic shock onset.
The Surviving Sepsis Campaign (SSC) recommends crystalloid and antimicrobial administration as soon as possible in patients with septic shock, but does not give clear guidelines on when to start vasopressors.1 Bai (2014) describes a 5.3% mortality increase for every one hour delay in norepinephrine initiation within six hours after septic shock onset.2
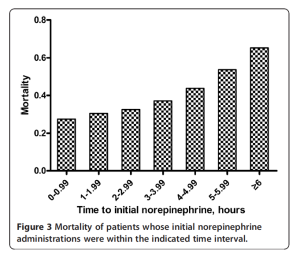
Avoid Pressor Angst! Ordering that 3rd and 4th liter of fluid is an easy trap to fall into, but remember — 20-30cc/kg is usually no more than 2L of crystalloid. Excessive fluid administration often delays adjunctive intervention, can prolong the duration of hypotension, and may cause significant morbidity. We discuss “Pressor angst” as the mental hurdle that prevents a clinician from prescribing vasoactive therapy, often because it will define a patient as “critically ill” and increase the amount of resources they will require (central venous catheter placement, increased monitoring, and higher level of care at disposition). The patient likely needs these interventions, not an additional liter of crystalloid…
Don’t delay vasoactives for central line placement. There is a growing body of evidence that peripheral vasoactive medication administration is safe3 It is appropriate to begin vasoactive medication peripherally early during resuscitation and then reassess the need for it after adequate fluid resuscitation, as opposed to delaying vasopressor therapy.[/x_accordion_item][/x_accordion][/x_column][/x_row][/x_section][x_section style=”margin: 0px 0px 0px 0px; padding: 0px 0px 0px 0px; “][x_row inner_container=”true” marginless_columns=”false” bg_color=”” style=”margin: 0px auto 0px auto; padding: 0px 0px 0px 0px; “][x_column bg_color=”” type=”1/1″ style=”padding: 0px 0px 0px 0px; “][x_text]
What’s your contingency pressor if your NE doses are escalating?
[/x_text][x_accordion][x_accordion_item title=”Answer” open=”false”]Pearl: Consider using your bedside echocardiogram to guide your choice of a 2nd line pressor
Cardiac dysfunction has been found to occur in 40-60% of patients with septic shock.4
The most recent SSC guidelines suggest the use of either epinephrine or vasopressin as a 2nd line vasopressors for septic shock. Epinephrine has more inotropic properties than norepinephrine, and is likely to be of particular benefit to the patients who have an associated cardiomyopathy.
Vasopressin in addition to norepinephrine (recommended to be run at .03 units/minute, not titrated) is believed to be beneficial due to a relative vasopressin deficiency associated with sepsis.
![Suggested starting point for vasoactives & inotropes for the patient with septic shock. [JCG]](https://penn.ccproject.com/wp-content/uploads/sites/8/2015/08/Sepsis-pressor-algorithm-300x203.jpg)
What are some of your resuscitation end-points in the patient with septic shock?
[/x_text][/x_column][/x_row][x_row inner_container=”true” marginless_columns=”false” bg_color=”” style=”margin: 0px auto 0px auto; padding: 0px 0px 0px 0px; “][x_column bg_color=”” type=”1/1″ style=”padding: 0px 0px 0px 0px; “][x_accordion][x_accordion_item title=”Answer” open=”false”]Pearl: A goal of a MAP of 65mmHg is recommended by the Surviving Sepsis campaign, but MAP does not guarantee perfusion. Aggressively monitor urine output, mental status, and skin perfusion to ensure adequate resuscitation
Having a general target of a MAP of 65 is a good place to start right up front, but additional factors should be considered. A baseline hypertensive patient may require a higher MAP to achieve adequate microperfusion, while an otherwise healthy, younger patient may be able to tolerate lower mean pressures. Urine output ( > 0.5 cc/kg/hr), mental status, and skin perfusion are important clinical findings to suggest adequate perfusion after the patient’s macrocirculatory goals are being met.
[/x_accordion_item][/x_accordion][/x_column][/x_row][/x_section][x_section bg_color=”#f4f4f4″ style=”margin: 0px 0px 0px 0px; padding: 0px0 0px 0 0px; border-style: solid; border-width: 1px 1px 1px 1px; border-color: #a0a0a0; “][x_row inner_container=”true” marginless_columns=”false” bg_color=”” style=”margin: 0px auto 0px auto; padding: 0px 0px 0px 0px; “][x_column bg_color=”” type=”1/1″ style=”padding: 0px 0px 0px 0px; “][x_text]References & Suggested Reading
- Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41(2):580-637. [PubMed Link]
- Bai X, Yu W, Ji W, et al. Early versus delayed administration of norepinephrine in patients with septic shock. Critical Care. 2014;18(5):532. [PubMed Link]
- Loubani OM, Green RS. A systematic review of extravasation and local tissue injury from administration of vasopressors through peripheral intravenous catheters and central venous catheters. J Crit Care. 2015; 30(3):653e9-653e17. [PubMed Link]
- Vieillard-baron A, Caille V, Charron C, Belliard G, Page B, Jardin F. Actual incidence of global left ventricular hypokinesia in adult septic shock. Crit Care Med. 2008;36(6):1701-6. [PubMed Link]
[/x_text][/x_column][/x_row][/x_section]