[cs_section id=”” class=” ” style=”margin: 0px; padding: 25px 0px 0px; border-style: ridge; border-width: 0px; border-width: 1px; ” visibility=”” parallax=”false”][cs_row id=”” class=” ” style=”margin: 0px auto; padding: 0px; ” visibility=”” inner_container=”true” marginless_columns=”false” bg_color=”” marginlesscolumns=””][cs_column id=”” class=”” style=”padding: 0px; ” bg_color=”” fade=”false” fade_animation=”in” fade_animation_offset=”45px” fade_duration=”750″ type=”1/1″][cs_text id=”” class=”” style=”” text_align=”none”]Author: Dr. Kathleen Lee
Reviewer & Edits: Dr. John Greenwood[/cs_text][/cs_column][/cs_row][/cs_section][cs_section id=”” class=” ” style=”margin: 0px; padding: 0px 0px 0; ” visibility=”” parallax=”false”][cs_row id=”” class=” ” style=”margin: 0px auto; padding: 0px; ” visibility=”” inner_container=”true” marginless_columns=”false” bg_color=”” marginlesscolumns=””][cs_column id=”” class=”” style=”padding: 0px; ” bg_color=”” fade=”false” fade_animation=”in” fade_animation_offset=”45px” fade_duration=”750″ type=”1/1″][cs_text id=”” class=”” style=”” text_align=”none”]
Clinical Case
45 year old male with past medical history of hemoglobin SS disease, congestive heart failure, pulmonary hypertension on 3L home oxygen, chronic kidney disease and chronic venous stasis ulcers who presents to the emergency department with altered mental status, shortness of breath and diffuse pain.
Initial laboratory values reveal worsening hepatic and renal function.
Initial Vitals:
T 98.6 F HR 123 BP 111/75 mmHg RR 29 SpO2 79% on 3L NC
The patient is lethargic & in mild respiratory distress. After completing your exam and reviewing the patient’s diagnostic labs, you suspect acute multiorgan dysfunction syndrome (MODS) due to his sickle cell crisis.[/cs_text][/cs_column][/cs_row][/cs_section][cs_section id=”” class=” ” style=”margin: 0px; padding: 0px; ” visibility=”” parallax=”false”][cs_row id=”” class=” ” style=”margin: 0px auto; padding: 0px; ” visibility=”” inner_container=”true” marginless_columns=”false” bg_color=”” marginlesscolumns=””][cs_column id=”” class=”” style=”padding: 0px; ” bg_color=”” fade=”false” fade_animation=”in” fade_animation_offset=”45px” fade_duration=”750″ type=”1/1″][cs_text id=”” class=”” style=”” text_align=”none”]
What is Acute Multiorgan Dysfunction Syndrome (MODS) in sickle cell patients?
[/cs_text][/cs_column][/cs_row][cs_row id=”” class=” ” style=”margin: 0px auto; padding: 0px; ” visibility=”” inner_container=”true” marginless_columns=”false” bg_color=”” marginlesscolumns=””][cs_column id=”” class=”” style=”padding: 0px; ” bg_color=”” fade=”false” fade_animation=”in” fade_animation_offset=”45px” fade_duration=”750″ type=”1/1″][x_accordion][x_accordion_item title=”Answer” open=”false”]Acute multiorgan dysfunction syndrome (MODS) is a severe and life threatening complication involving the dysfunction of at least two of three major organs in the setting of a sickle pain episode. The development of MODS during an episode of sickle cell pain crisis has been associated with sepsis, fat embolism, and has also occurred with no associated conditions in some fatal cases.
Specific diagnostic criteria include:
Lung
- Acute pulmonary infiltrate
- Hypoxia requiring > 3L of oxygen
Liver
- ALT level >5x normal and baseline values
- Total bilirubin level > 5x normal and baseline values
- Direct bilirubin level > 2x normal and baseline values
- Prothrombin time > 3 seconds prolonged
Kidney
- Acute elevate of serum creatinine > 2.0 mg/dL
[/x_accordion_item][/x_accordion][/cs_column][/cs_row][/cs_section][cs_section id=”” class=” ” style=”margin: 0px; padding: 0px; ” visibility=”” parallax=”false”][cs_row id=”” class=” ” style=”margin: 0px auto; padding: 0px; ” visibility=”” inner_container=”true” marginless_columns=”false” bg_color=”” marginlesscolumns=””][cs_column id=”” class=”” style=”padding: 0px; ” bg_color=”” fade=”false” fade_animation=”in” fade_animation_offset=”45px” fade_duration=”750″ type=”1/1″][cs_text id=”” class=”” style=”” text_align=”none”]
Why do patients with SSD develop acute MODS?
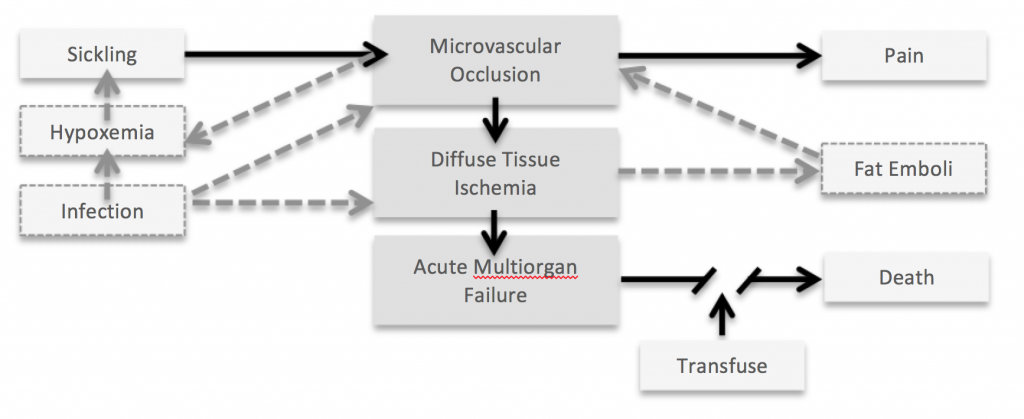
[/cs_text][x_accordion][x_accordion_item title=”Answer” open=”false”]One hypothesis regarding the pathophysiology of acute MODS in SSD suggests that the diffuse sickling that occurs during a severe vaso-occlusive pain episode leads to diffuse tissue ischemia resulting in acute multiorgan failure. Additional factors that may precipitate this chain of events include infection, hypoxemia and fat emboli.
[/x_accordion_item][/x_accordion][/cs_column][/cs_row][/cs_section][cs_section id=”” class=” ” style=”margin: 0px; padding: 0px; ” visibility=”” parallax=”false”][cs_row id=”” class=” ” style=”margin: 0px auto; padding: 0px; ” visibility=”” inner_container=”true” marginless_columns=”false” bg_color=”” marginlesscolumns=””][cs_column id=”” class=”” style=”padding: 0px; ” bg_color=”” fade=”false” fade_animation=”in” fade_animation_offset=”45px” fade_duration=”750″ type=”1/1″][cs_text id=”” class=”” style=”” text_align=”none”]
What type of venous access will you need for exchange transfusion?
[/cs_text][x_accordion][x_accordion_item title=”Answer” open=”false”]Pearl: Peripheral IV access is generally adequate for apheresis red cell exchange.
Many venous access devices do not support the flow rates required by apheresis machines. Although the data is limited, temporary hemodialysis catheters, vortex ports and double or dual ports may be used.[/x_accordion_item][/x_accordion][/cs_column][/cs_row][/cs_section][cs_section id=”” class=” ” style=”margin: 0px; padding: 0px; ” visibility=”” parallax=”false”][cs_row id=”” class=” ” style=”margin: 0px auto; padding: 0px; ” visibility=”” inner_container=”true” marginless_columns=”false” bg_color=”” marginlesscolumns=””][cs_column id=”” class=”” style=”padding: 0px; ” bg_color=”” fade=”false” fade_animation=”in” fade_animation_offset=”45px” fade_duration=”750″ type=”1/1″][cs_text id=”” class=”” style=”” text_align=”none”]
What are some of your resuscitation end-points in the patient with SSD associated MODS?
[/cs_text][/cs_column][/cs_row][cs_row id=”” class=” ” style=”margin: 0px auto; padding: 0px; ” visibility=”” inner_container=”true” marginless_columns=”false” bg_color=”” marginlesscolumns=””][cs_column id=”” class=”” style=”padding: 0px; ” bg_color=”” fade=”false” fade_animation=”in” fade_animation_offset=”45px” fade_duration=”750″ type=”1/1″][x_accordion][x_accordion_item title=”Answer” open=”false”]Pearl: Simple transfusions of normal red blood cells to patients with SCD lead to an increase in blood viscosity, which can paradoxically worsen end-organ perfusion.
Early recognition of this syndrome and the initiation of transfusion therapy can be life-saving.
However, simple transfusions of normal red blood cells to patients with SCD lead to an increase in blood viscosity, which can paradoxically worsen end-organ perfusion. The relatively high baseline hemoglobin concentrations are seen in MODS point to viscosity as a major contributor. Accordingly, red cell exchange is nearly always the treatment of choice in MODS. Goals of transfusion are to reduce the sickle cell fraction to less than 30% HbS for HbSS or 15% HbS HbSC.
- Red cell volume = hematocrit × total blood volume.
- Assume total blood volume is 70 cc/kg if over 20 kg,
85 cc/kg if under 20 kg. - Each standard unit has a red cell volume of ~200 cc
(Hct ~40 × 500 cc)
- Assume total blood volume is 70 cc/kg if over 20 kg,
- Calculate exchange volume as 1.5 red cell volumes.
[/x_accordion_item][/x_accordion][/cs_column][/cs_row][/cs_section][cs_section id=”” class=” ” style=”margin: 0px; padding: 0px0 0px 0; border-style: solid; border-width: 0px; border-width: 1px; border-color: #a0a0a0; ” visibility=”” bg_color=”#f4f4f4″ parallax=”false”][cs_row id=”” class=” ” style=”margin: 0px auto; padding: 0px; ” visibility=”” inner_container=”true” marginless_columns=”false” bg_color=”” marginlesscolumns=””][cs_column id=”” class=”” style=”padding: 0px; ” bg_color=”” fade=”false” fade_animation=”in” fade_animation_offset=”45px” fade_duration=”750″ type=”1/1″][cs_text id=”” class=”” style=”” text_align=”none”]References & Suggested Reading
- Hassell KL, Eckman JR, Lane PA. Acute multiorgan failure syndrome: a potentially catastrophic complication of severe sickle cell pain episodes. Am J Med. 1994;96(2):155-62. [PubMed Link]
- Swerdlow PS. Red cell exchange in sickle cell disease. Hematology Am Soc Hematol Educ Program. 2006;48-53. [PubMed Link]
- Fasika M Tedla, Eli A Friedman. Multiorgan failure during a sickle cell crisis in sickle +– beta thalassemia. American J of Kidney Diseases. Vol 42(2); e4.1-e4.3.
[/cs_text][/cs_column][/cs_row][/cs_section]